Payors
HealtFAXTM is your digital navigator for healthcare, Personalized communications with clinics, labs, and payors, Access high-grade medical information instantly, Your entire healthcare journey with HealtFAXTM

Provide your members an easy way to understand their health plans, obtain test cost estimates and review the status of their health plans all from HealthFAX™.
Member satisfaction is the key for member retention and with HealthFAX™ members can conversationally provide information and get accurate answers. HealthFAX™ has a rich Natural Language Understanding empowering members to converse with their health plan.
Convert any process into a conversational experience for your members instantly with HealthFAX™ and drive revenues, reduce the burden on your staff and gain productivity.
Educate your members about your insurance plans and benefits with HealthFAX™ KnowledgeBOT. The KnowledgeBOT has more than 2 million questions and answers and users ask questions conversationally.
Eliminate member anxiety and provide members with the information they need about their healthcare costs, instantly, with HealthFAX™ in a conversational manner.
Reduce the burden on your staff by allowing HealthFAX™ to answer questions and provide real-time test cost estimates and detailed snapshots of a member’s health insurance such as co-pay, deductibles, co-insurance, etc.
Health insurance education is available with HealthFAX™ KnowledgeBOT.
Provide your members the ease to their healthcare journey by regular follow-up based on their health plans via HealthFAX™. During follow-up, HealthFAX™ will follow through with members about their recovery process and suggesting the next steps.
Use HealthFAX™ ExpertConnect to immediately connect your members to experts via a live chat or scheduled phone call.

Provide information about health plans instantly & efficiently.

Directing members to the most relevant and cost-effective medical providers.

Real-time test cost estimations.

Learn about health insurance by asking questions in natural language.

Empower providers with the tools they need for health insurance claims processing. HealthFAX™ collects patient information conversationally and provides a complete patient profile thereby reducing claim denials.
HealthFAX™ automates the entire process of pre-authorization documentation and prepares it for transmitting it to your network for processing, reducing bottlenecks, and enhancing process optimization.
Payors and members can check claim statuses with HealthFAX™ chatbots and ask any questions to HealthFAX™ KnowledgeBOT.
HealthFAX™ simplifies the revenue life cycle management by meaningfully connecting all the stakeholders.

Proactively collecting patient information pre-visit.

Reducing claims denials by generating accurate information.

Automating RCM processes such as prior authorizations.

Live connect with Health Experts for complex situations.
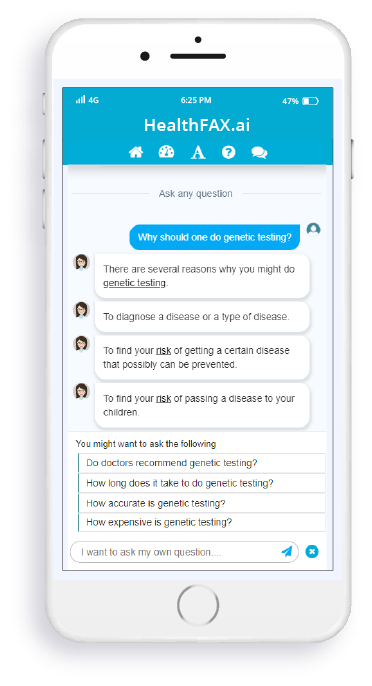
More than 2 million curated questions & answers
Instantly educate members about health insurance
Empower members to ask questions in natural language
Review contextually relevant information instantly